By Dave DeFusco
When doctors look at images of the human brain, they are searching for tiny signs that can mean the difference between life and death. A shadow in the wrong place, a shape that does not belong or a slight change in texture can signal a brain tumor. Finding those signs early is critical, but it is also incredibly difficult. The brain is complex, and tumors can hide in ways that even experienced specialists may struggle to see.
For Puspita Chowdhury, a student in the Katz College’s M.S. in Artificial Intelligence, this challenge is not only scientific, it is personal. As a child, Chowdhury lost her uncle to a brain tumor. By the time doctors understood what was happening, the disease had already reached a critical stage. He died young, leaving behind a small son and a grieving family. Years later, that loss has stayed with her.
“Someone in my family going through this made me want to understand why brain tumors are so hard to detect and why they are often found too late,” said Chowdhury. “I wanted to see if technology could help doctors find them earlier, before it becomes critical.”
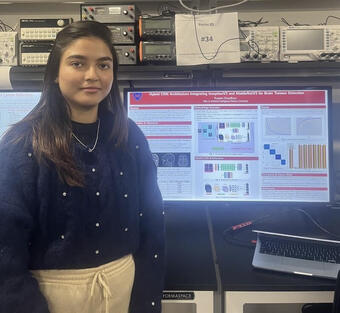
That motivation led to her research project, “Hybrid CNN Architecture Integrating InceptionV3 and MobileNetV3 for Brain Tumor Detection,” which she presented recently at the Stevens Institute of Technology. While the name sounds technical, the goal is simple: help doctors identify brain tumors faster and more accurately using computer assistance.
Chowdhury’s work focuses on MRI scans, which are images doctors already use to examine the brain. She designed a computer system that looks at these images and sorts them into four categories: glioma, meningioma, pituitary tumor and normal. These tumor types can look very similar, even to trained eyes, especially in early stages.
“Brain tumors don’t always have clear borders,” she said. “Their shapes, sizes and locations can overlap, and that makes diagnosis very challenging for both humans and computers.”
To tackle this problem, Chowdhury combined two different computer models. One, called InceptionV3, is very good at noticing fine details such as shape and structure. The other, MobileNetV3, works faster and is more efficient. On their own, each had weaknesses. Together, they balanced each other.
“InceptionV3 gives very strong accuracy but can become too focused on the training data,” said Chowdhury. “MobileNetV3 is fast, but not always detailed enough. By combining them, one helps with precision and the other with speed.”
She trained her system using 3,762 MRI images from a public dataset. To help the computer learn better, she carefully prepared the images by resizing them, adjusting brightness and creating slightly altered versions, such as rotated or flipped images, but only for training. This step was crucial to avoid “data leakage,” a problem that can make results seem better than they truly are.
“In medical research, fairness matters,” said Chowdhury. “If the system sees test images during training, it can give false confidence. I made sure the test data stayed completely separate.”
The result was striking. The hybrid system achieved 98.1% accuracy, outperforming single-model approaches. More important, it reduced false negatives—cases where a tumor exists but is missed. In healthcare, missing a tumor can delay treatment and cost lives.
Jiang Zhou, a professor in the master’s in AI, emphasized the importance of that achievement. “The real value of this research is not just the high accuracy,” he said. “It’s the reduction of missed cases and the balanced performance across different tumor types. That’s what makes it meaningful for clinical decision support.”
Chowdhury doesn’t see her work as replacing doctors. Instead, she envisions it as a supportive tool that helps radiologists focus their attention and save time.
“My model is not here to replace medical professionals,” she said. “It’s here to help them quickly understand where the tumor might be, so they can plan surgery or treatment more effectively. If this kind of tool can help even one family avoid what mine went through, then the work is worth it.”